The importance of OR efficiency
In the current environment the pressure on healthcare providers has never been greater.
Maximising the efficiency of their assets so that they can meet the ever-increasing demand for higher quality, more cost-effective provision of services is paramount.
The Covid pandemic has highlighted how delicate a balance most healthcare systems have when it comes to asset utilisation. The vast majority cannot afford any kind of operational slack, where a buffer of excess resources exists in the system that provides the ability to cope with transient increases in demand, whether they are predicted (such as seasonal illness) or not (the Covid pandemic). Most are at the opposite end of the spectrum, with labour shortages and aging infrastructure leading to a long-term, fire-fighting mode of operation. In many countries, the pandemic threatens to both highlight and accelerate what many have predicted in recent years: under-investment leading to the erosion in the quantity and quality of healthcare services, with an inevitable impact on patient care.
Within the hospital, the operating room is among the most important areas of the hospital, because it is a major determinant of both the workload and the revenue. Efficient use of OR time depends on many factors. Scheduling of cases, allocation of resources (staff and equipment), preparation and induction of anaesthesia, performance of the procedure, patient recovery, and preparation of the OR for the next procedure must all work in co-ordination. An unanticipated delay in any one or more of these steps is disruptive and affects the synchrony of this complex chain of events. With so many interacting pieces to this puzzle, it does not take much to cause significant delay.
An inefficient OR can result in case cancellations and long patient waiting lists. In contrast, a well-managed OR results not only in a high surgical turnover, but also in reduced postoperative complications, improved patient-centred outcomes, and greater patient satisfaction[i]. Several performance parameters influencing OR utilization have been reported[ii]. These include accurate estimation of the duration of the procedure; the percentage of on-time first case starts; the performance of pre-admission screening procedures; patient-in-to-first incision time; and average turnover time between patients.
Operating rooms are expensive to run, with every minute wasted having an opportunity cost where a procedure could be performed that (in most healthcare systems) earns revenue for the hospital. In the UK, OR costs have been estimated at £1,200 per hour and, in one study, an improvement in patient operating room contact time of 10% yielded an annual efficiency saving for the hospital of £3.2m per year [iii]. Costs in the US are even higher, with a study of 100 U.S. hospitals found that OR charges averaged $62 per minute ($3,720 per hour)[iv].
Delays in laparoscopic surgery
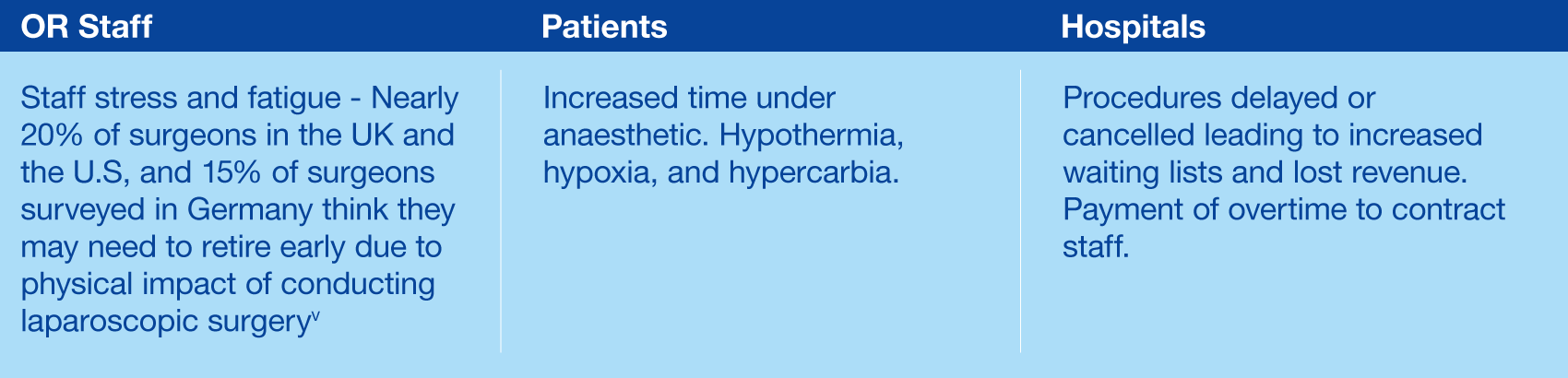
Laparoscopic surgery has proven, demonstrable benefits for patients. However, inefficiencies and prolonged surgery times have consequences for all stakeholders involved:
[i] JV Divatia and P Ranganathan (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4944359/)
[ii] Foster
(https://www.ormanager.com/wp-content/uploads/2012/01/0112_ORM_5.Benchmark_r.pdf)
[iii] NHS Institution for Innovation and Improvement. “Improving quality and efficiency in the operating theatre”
[iv] Shippert (https://journals.sagepub.com/doi/10.1177/074880680502200104)
[v] CMR Surgical survey (https://cmrsurgical.com/news/one-in-five-surgeons-set-to-retire-early-due-to-physical-toll)
